The Age of Health Informatics: Part 1

Introduction
In the digital transformation era, healthcare is experiencing a paradigm shift driven by integrating data science, machine learning, and information technology. This article explores the profound impact of health informatics, focusing on data scientists and machine learning engineers who play a pivotal role in leveraging data-driven approaches to revolutionize healthcare. We will examine real-life applications where health informatics has outperformed traditional methods, discuss recent advances in the field, and highlight machine learning tools such as time series analysis with ARIMA and ARTXP that are transforming health informatics.
The Role of Data Scientists and ML Engineers in Health Informatics
At the heart of the Age of Health Informatics are data scientists and ML engineers who play a critical role in harnessing the power of data and developing intelligent algorithms. These professionals apply their expertise to analyze large and complex healthcare datasets, extract meaningful insights, build predictive models, and create innovative solutions that drive evidence-based decision-making and enhance patient outcomes.
Here are some critical contributions of data scientists and machine learning engineers in health informatics:
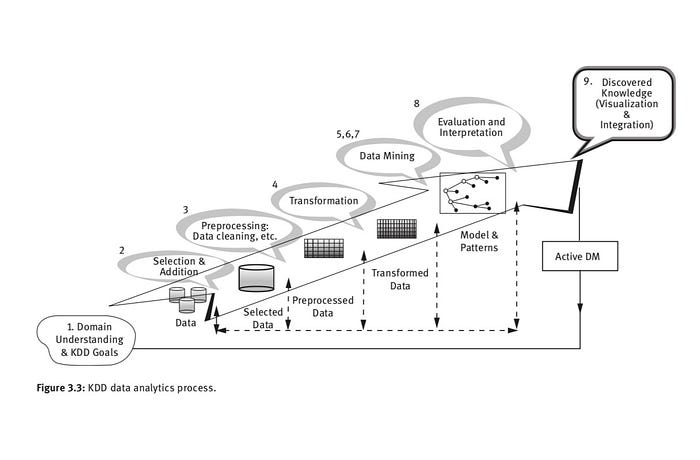
- Data Analysis and Visualization: Data scientists and machine learning engineers are skilled in analyzing large, complex healthcare datasets. They employ advanced statistical techniques, data mining, and visualization tools to uncover patterns, trends, and correlations within the data. They can identify factors influencing disease outcomes, treatment responses, and population health trends by understanding the relationships between various healthcare variables.
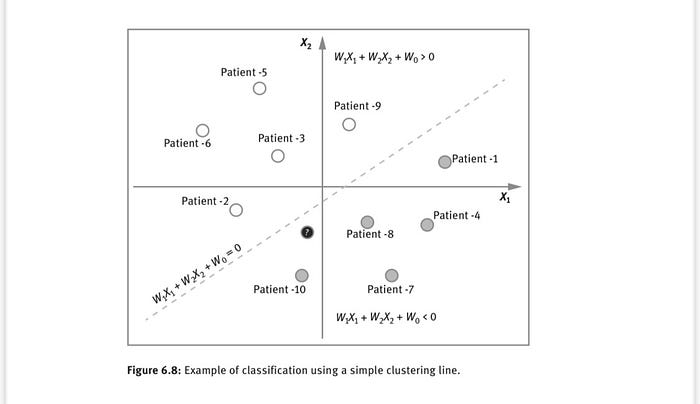
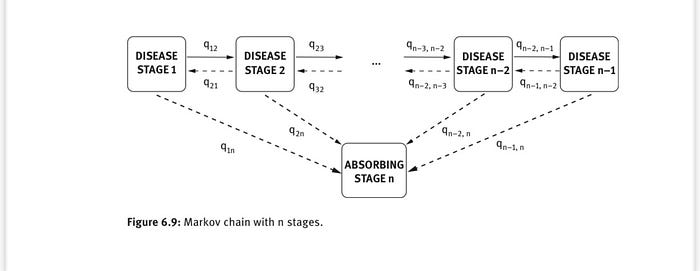
- Predictive Modeling and Risk Stratification: They also develop predictive models to forecast disease progression and patient outcomes and identify high-risk individuals for developing specific health conditions. By analyzing historical data and utilizing predictive machine learning algorithms like BERT, ARIMA, Markov Chain Analysis, Principal Component Analysis, and Support Vector Machine, they can assess the likelihood of adverse events, such as hospital readmissions, and stratify patients based on risk profiles. This information aids in early interventions, personalized treatment plans, and resource allocation.
- Image and Signal Processing: In medical imaging and signal processing, data scientists and machine learning engineers employ advanced algorithms to extract valuable information from images, such as CT scans, MRIs, and EKGs. By utilizing techniques like computer vision and deep learning, they can detect abnormalities, assist in disease diagnosis, and provide quantitative measurements. These technologies help radiologists and clinicians accurately and efficiently interpret medical images, improving diagnostic accuracy and treatment planning.
- Natural Language Processing (NLP) and Text Mining: Healthcare data includes vast amounts of unstructured information in clinical notes, research articles, and patient narratives. Data scientists and machine learning engineers employ NLP techniques and text-mining algorithms to process and analyze this textual data. By extracting meaningful insights from unstructured clinical text, they can automate coding, identify adverse events, and assist in clinical decision-making. NLP also enables efficient information retrieval, literature reviews, and evidence-based medicine.
- Data Integration and Interoperability: Healthcare data exists in various formats and systems, making interoperability a significant challenge. Data scientists and machine learning engineers work on integrating diverse data sources, such as electronic health records, wearable devices, and genomics data. Developing data integration frameworks enables seamless data exchange, aggregation, and analysis, providing a comprehensive view of the patient’s health status and supporting personalized medicine initiatives.
- Algorithm Development and Validation: Data scientists and machine learning engineers are responsible for developing and validating algorithms that power health informatics applications. They employ rigorous validation processes, including cross-validation, performance evaluation, and benchmarking, to ensure the developed algorithms’ accuracy, reliability, and generalizability. By continuously refining and optimizing algorithms, they improve health informatics applications’ precision, sensitivity, and specificity.
- Ethical Considerations and Bias Mitigation: Data scientists and ML engineers play a vital role in addressing ethical considerations and mitigating biases in health informatics. They evaluate algorithms’ fairness, transparency, and accountability to ensure equitable and unbiased healthcare practices. By incorporating ethical frameworks, promoting algorithmic transparency, and implementing bias-mitigation techniques, they contribute to the responsible and ethical use of data and technology in healthcare.
Data scientists and machine learning engineers bring valuable skills and expertise to the field of health informatics. Their contributions in data analysis, predictive modelling, image processing, NLP, data integration, algorithm development, and ethical considerations are instrumental in harnessing the power of healthcare data and advancing the field to improve patient care, outcomes, and population health.
Real-Life Applications
Health informatics has demonstrated its transformative potential in various real-life applications, showcasing its superiority over traditional approaches. For instance, machine learning algorithms have proven more accurate and efficient in disease diagnosis than manual interpretation of medical images. Computer-aided detection and diagnosis systems utilizing deep learning models have shown remarkable performance in detecting abnormalities in radiology scans, such as mammograms for breast cancer detection or retinal images for diabetic retinopathy screening. These technologies have the potential to enhance early detection and improve patient outcomes.
Another notable application is predictive analytics in healthcare. Researchers and practitioners can develop models that predict patient outcomes, risk stratification, and disease progression by leveraging machine learning techniques on large-scale healthcare datasets. For example, predictive models based on electronic health records can assist in identifying patients at high risk of developing complications, enabling timely interventions and personalized treatment plans. These data-driven approaches could revolutionize healthcare delivery and improve patient care.

Advances in Health Informatics
The field of health informatics has witnessed significant advances driven by rapid developments in data science and machine learning. One prominent area is using natural language processing (NLP) techniques to extract valuable information from unstructured clinical text, such as physician notes or medical literature. NLP algorithms can process and analyze vast amounts of text data, enabling automated coding, clinical decision support, and efficient information retrieval.
Another exciting advancement is the integration of genomic and clinical data. The emergence of precision medicine has led to the generation of extensive genomic datasets, requiring sophisticated computational approaches for analysis and interpretation. Machine learning algorithms are deployed to uncover disease-associated genetic markers, predict drug responses, and facilitate personalized treatment strategies.
Machine Learning Tools for Health Informatics
Machine learning is vital in health informatics, offering powerful tools to extract insights from complex healthcare data. Time series analysis is one such tool with extensive application in health informatics. Methods like Autoregressive Integrated Moving Average (ARIMA) are widely used to analyze temporal patterns and make predictions based on historical data. Time series analysis helps forecast disease outbreaks, patient readmissions, and treatment responses, enabling proactive interventions and resource allocation.
Another notable machine learning tool is the ARTXP algorithm, an advanced regression tree-based method. ARTXP combines the advantages of regression trees and statistical modeling to handle complex, non-linear relationships in healthcare data. It offers improved interpretability, allowing researchers and clinicians to understand the factors contributing to specific outcomes and make informed decisions. ARTXP has been applied in various healthcare domains, including predicting hospital readmissions, identifying high-cost patients, and personalized risk assessment.

Challenges in Health Informatics
Despite its transformative potential, health informatics also faces various challenges that must be addressed for successful implementation and advancement. Here are some critical challenges in health informatics:
- Data Quality and Interoperability: Health informatics relies heavily on accurate and comprehensive data. However, ensuring data quality can be a significant challenge. Data may be inconsistent, incomplete, or stored in various formats across different systems. Achieving interoperability among disparate healthcare systems, including electronic health records (EHRs), imaging systems, and laboratory databases, is essential for seamless data exchange and effective collaboration. Standardization of data formats, coding systems, and communication protocols is necessary to overcome these challenges.
- Privacy and Security: Health information is highly sensitive and subject to strict privacy regulations. Protecting patient privacy and ensuring data security are paramount in health informatics. Data breaches and unauthorized access can lead to severe consequences, including identity theft and compromised patient safety. Implementing robust security measures, encryption techniques, access controls, and complying with privacy regulations such as HIPAA (Health Insurance Portability and Accountability Act) is important for maintaining the confidentiality and integrity of health data.
- Data Governance and Ethics: Health informatics deals with a vast amount of data, and ethical considerations must guide its collection, storage, analysis, and use. Issues such as informed consent, data ownership, and responsible data sharing must be carefully addressed to maintain public trust. Developing clear data governance policies and ethical frameworks that ensure transparency, fairness, and accountability in data handling is essential.
- Integration of New Technologies: Health informatics must adapt to technologies like artificial intelligence, machine learning, and Internet of Things devices. Incorporating these technologies into existing healthcare systems requires careful planning, technical expertise, and consideration of ethical implications. The challenge lies in seamlessly integrating these technologies, training healthcare professionals to utilize them effectively, and ensuring their reliability and safety in clinical practice.
- Workforce Education and Training: Health informatics requires a skilled workforce capable of effectively utilizing data science, analytics, and technology. There is a need for specialized training programs and educational initiatives to equip healthcare professionals, data scientists, and machine learning engineers with the necessary knowledge and skills in health informatics. Bridging the gap between traditional healthcare disciplines and data science is crucial to fully harness the potential of health informatics.
- Change Management and Adoption: Implementing health informatics solutions often involves significant organizational and cultural changes. Resistance to change, lack of buy-in from stakeholders, and limited financial resources can impede the adoption of health informatics initiatives. Effective change management strategies, leadership support, and a culture that values innovation and data-driven decision-making are essential to overcome these challenges.
- Ethical Use of AI and Machine Learning: With the increasing use of AI and machine learning in health informatics, ethical concerns arise regarding bias, transparency, and accountability. Addressing algorithmic fairness, interpretability, and potential biases in training data is crucial to ensuring equitable and responsible use of these technologies. Developing guidelines, standards, and regulatory frameworks that promote ethical AI and machine learning practices is vital.
Addressing these challenges requires collaborative efforts among stakeholders, including healthcare organizations, policymakers, researchers, and technology developers. By addressing data quality, privacy, governance, education, and ethical considerations, we can unlock the full potential of health informatics and drive positive transformations in healthcare delivery and patient outcomes.
Conclusion
The Age of Health Informatics presents unprecedented opportunities for revolutionizing the healthcare industry. Through real-life applications, we have witnessed the superiority of health informatics over traditional methods, offering enhanced accuracy, efficiency, and personalized care. Recent advances in the field and machine learning tools like time series analysis with ARIMA and ARTXP have further propelled health informatics into new frontiers. By harnessing the power of ML, health informatics can transform and pave the way for a more data-driven and patient-centered approach to medicine.